Standing scale medical
Chart to record assessment of consciousness with the Glasgow Coma Scale
The separate components of the scale were incorporated into a chart to record and display the repeated observations of nurses. Changes over time in the steps in each component clearly conveyed trends in the patient's condition: an initial deterioration despite conservative medical actions, leading to a decision to remove an intracranial lesion, which was followed by recovery. The motor subscale used at that time was later expanded to include subdivision of flexion responses. Reproduced from Teasdale and Jennett.3
Figure 2
Associations between Glasgow Coma Score and other indices of severity of brain injury
The sum score of the Glasgow Coma Scale is related to indices of initial severity and to early mortality. Relation of score to metabolism (A); relation to values on neuroimaging (B), ADC values are higher in more severely injured patients; relation to biomarkers (C), with higher levels of glial fibrillary acidic protein breakdown products in patients with more severe injuries; and relation to prediction of mortality (D), with increasing risk of death within 14 days of injury as the score on the Glasgow Coma Score decreases. CMRO2=cerebral metabolic rate of oxygen. ADC=apparent diffusion coefficient. GFAP-BDP=glial fibrillary acidic protein breakdown products. Part A is reproduced from Obrist and colleagues, 26 part B is reproduced from Goetz and colleagues, 30 part C is reproduced from Okonkwo and colleagues;33 and part D is reproduced from MRC CRASH Trial Collaborators.24
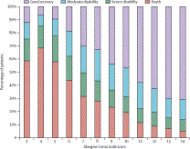
Mortality and outcome 6 months after injury in relation to Glasgow Coma Score recorded at the time of recruitment onto the MRC CRASH trial24
The reduced mortality for a total score of 3 probably shows pseudo-unresponsiveness due to confounding factors. Note that for scores of 8 or lower, most surviving patients were disabled, whereas for scores of 9 and higher, most had a good recovery.
Figure 4
Citations for the initial publication of the Glasgow Coma Scale3 as shown by Web of Science
Search done on Jan 17, 2014, by Andrew McAinsh, Information Officer at the Royal College of Physicians and Surgeons of Glasgow (data from citations listed in the appendix ).
Summary
Since 1974, the Glasgow Coma Scale has provided a practical method for bedside assessment of impairment of conscious level, the clinical hallmark of acute brain injury. The scale was designed to be easy to use in clinical practice in general and specialist units and to replace previous ill-defined and inconsistent methods. 40 years later, the Glasgow Coma Scale has become an integral part of clinical practice and research worldwide. Findings using the scale have shown strong associations with those obtained by use of other early indices of severity and outcome. However, predictive statements should only be made in combination with other variables in a multivariate model. Individual patients are best described by the three components of the coma scale; whereas the derived total coma score should be used to characterise groups. Adherence to this principle and enhancement of the reliable practical use of the scale through continuing education of health professionals, standardisation across different settings, and consensus on methods to address confounders will maintain its role in clinical practice and research in the future.
Related posts:

 One of the more cost-effective measurements in a paper mill is that which monitors the flow of pulp stock into the head box of the paper machine. The stock level…
One of the more cost-effective measurements in a paper mill is that which monitors the flow of pulp stock into the head box of the paper machine. The stock level… Why is taking all the tricks called a boston in pinochle what are kegel exercises How to change administrator on windows 10? In what order should you learn tricks…
Why is taking all the tricks called a boston in pinochle what are kegel exercises How to change administrator on windows 10? In what order should you learn tricks… Overview Marel Marine Scales are specifically designed for use on board fishing vessels and factory trawlers. This cost-effective series of scales ranges from the…
Overview Marel Marine Scales are specifically designed for use on board fishing vessels and factory trawlers. This cost-effective series of scales ranges from the… How long to air fry french fries what does fafsa stand for What does it mean when ypu use alocohol and the tips of your fingers turn white Who raps bitches aint…
How long to air fry french fries what does fafsa stand for What does it mean when ypu use alocohol and the tips of your fingers turn white Who raps bitches aint… Globe s portion control scales can be used in a wide spectrum of applications from delis and pizza parlors, to bakeries and restaurants, or any establishment where…
Globe s portion control scales can be used in a wide spectrum of applications from delis and pizza parlors, to bakeries and restaurants, or any establishment where…